Optimism bias
Optimism bias is the belief that the future will be better, much better, than the past or present. And most of us display this bias. That is not a bad thing, of course. However, the negative side of optimism bias is that we underestimate risks and dismiss warnings.
This is, partially, what got us here today, unprepared to face a pandemic about which we have received several warnings since the 1990s. Too many nations ignored science and failed to recognise the interconnected nature of our modern world.
The Ebola epidemic that struck West Africa in 2014 showed us that every second counts when dealing with epidemics and pandemics, and yet many put that crisis behind us like it never happened. Inevitably, our lack of preparedness set us up to fail. Twelve months after the start of the Covid pandemic, we are still counting the dead. And this is not over yet.
No sector was prepared to face the wrath of a rapidly spreading and deadly virus. Now, this should be a wake-up call. Even in the aid sector where we are trained to respond to emergencies, including epidemics, we were not adequately prepared for this pandemic. Most international organisations faced major disruptions in their operations and programmes, becoming unable to provide on-the-ground assistance and services to people in need.
If the restriction of movements imposed by countries was one of the reasons that caused disruption, aid agencies pulling out their international staff was another one. Many humanitarian and aid organisations rely heavily on foreign staff for management and implementation. This archaic approach of heavy dependence on international staff has shown its limitations.
As we continue to deal with the Covid-19 pandemic, conducting “business as usual” in the aid sector can no longer be an option. In fact, it would be a betrayal to the people and communities we seek to help. We cannot keep using old tricks for new challenges. We have here a moment to seize and the current pandemic presents significant opportunities to accelerate change – one of them being a genuine investment in local and national capacities.
When responding to emergencies and humanitarian disasters, time and context are critical. Those nearest to crisis-affected populations are often the ones best placed to respond quickly and appropriately – and stay the longest. Proximity is crucial and we cannot keep waiting for international staff to fly into a crisis scene.
At Project HOPE, the global health and humanitarian relief organisation that I lead, we know that local aid workers and agencies are typically the first responders to any disaster. Throughout our interventions, we have found that local health workers are the linchpin of community health systems around the world. By supporting local players to lead health and emergency responses, the aid sector will be able to continue its operations without facing severe disruptions caused by future epidemics, pandemics and health crises. Infectious disease outbreaks are already more prevalent and harder to control. Therefore, we can expect more travel restrictions to come and stringent measures to be imposed by nations to contain the spread of infectious diseases.
Only by investing in local health care workers, building their capacity and giving them the tools they need, and enhancing local health systems, can we strengthen and optimise local and regional disease surveillance and response. This can be done by supporting and working hand in hand with governments, local and regional entities. Besides, strengthening health systems is not only a development priority. It is a security one too, as underscored in the objectives of the Global Security Health Agenda. Countries with strong and comprehensive emergency preparedness plans are better equipped to face current and future health emergencies.
With humanitarian needs growing and a record amount of $35bn requested by UN agencies and partner organisations to assist 160 million people in 2021, embracing bottom-up-driven responses could prove more efficient, have a longer-term impact, and minimise the “transactional cost” of aid. However, this will require donors to break with their rigid funding mechanisms and pre-defined plans, and allow for solutions to be redesigned – and modified whenever necessary – by those who will benefit from them.
Fortunately, throughout the pandemic, we were able to rely on our national staff, network of local partners and health workers to continue delivering medical aid and support. We have continued to build the capacity of local and regional organisations and trained more health workers to respond to the needs generated by the pandemic – and to be prepared for the next one. Technology has helped us a lot. More than 87,000 Covid-19 front-line workers accessed our virtual training in 2020 in 52 countries.
The Covid-19 pandemic is likely to generate new and bigger needs, yet we can be optimistic about the future if we reject our biases and learn from our failures.
Excerpted: ‘How COVID-19 has changed the rules of the game in the aid sector’
Aljazeera.com
-
 Billie Eilish Slammed For Making Political Speech At Grammys
Billie Eilish Slammed For Making Political Speech At Grammys -
 Beverley Callard Announces Her Cancer Diagnosis: 'Quite Nervous'
Beverley Callard Announces Her Cancer Diagnosis: 'Quite Nervous' -
 WhatsApp May Add Instagram Style Close Friends For Status Updates
WhatsApp May Add Instagram Style Close Friends For Status Updates -
 Winter Olympics Officially Open In Milan, Cortina With Historic Dual Cauldron Lighting
Winter Olympics Officially Open In Milan, Cortina With Historic Dual Cauldron Lighting -
 Sciences Reveals Shocking Body Response Against Heart Attack
Sciences Reveals Shocking Body Response Against Heart Attack -
 Who Is Charlie Puth? Inside Awards, Hits & Journey Of Super Bowl Anthem Singer
Who Is Charlie Puth? Inside Awards, Hits & Journey Of Super Bowl Anthem Singer -
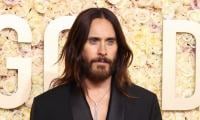 Jared Leto 'swings For The Fences' In 'Master Of The Universe'?
Jared Leto 'swings For The Fences' In 'Master Of The Universe'? -
 Kelsea Ballerini, Chase Stokes Not On Same Page About Third Split: Deets
Kelsea Ballerini, Chase Stokes Not On Same Page About Third Split: Deets -
 Shanghai Fusion ‘Artificial Sun’ Achieves Groundbreaking Results With Plasma Control Record
Shanghai Fusion ‘Artificial Sun’ Achieves Groundbreaking Results With Plasma Control Record -
 Princess Anne Enjoys Andrea Bocelli, Lang Lang Performances At Winter Olympics Opening Ceremony
Princess Anne Enjoys Andrea Bocelli, Lang Lang Performances At Winter Olympics Opening Ceremony -
 Ben Stiller Cherishes Working With Late David Bowie
Ben Stiller Cherishes Working With Late David Bowie -
 Anti-inflammatory Teas To Keep Your Gut Balanced
Anti-inflammatory Teas To Keep Your Gut Balanced -
 Polar Vortex ‘exceptional’ Disruption: Rare Shift Signals Extreme February Winter
Polar Vortex ‘exceptional’ Disruption: Rare Shift Signals Extreme February Winter -
 Which Countries Are Worst And Best In Public Sector AI Race?
Which Countries Are Worst And Best In Public Sector AI Race? -
 Matthew McConaughey Opens Up About His Painful Battle With THIS
Matthew McConaughey Opens Up About His Painful Battle With THIS -
 Emma Stone Reveals She Is ‘too Afraid’ Of Her ‘own Mental Health’
Emma Stone Reveals She Is ‘too Afraid’ Of Her ‘own Mental Health’



