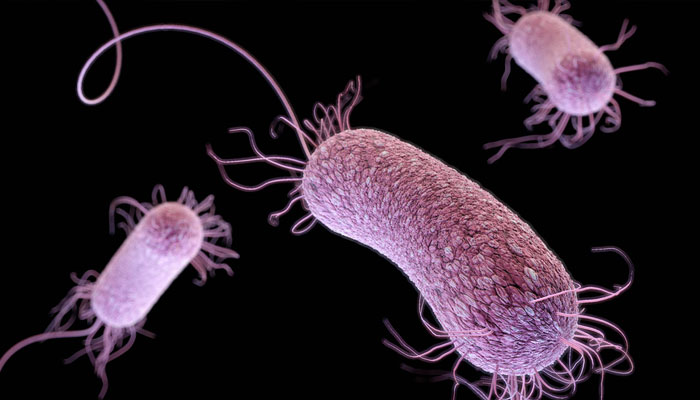
Beware the superbug
Medical experts estimate that global deaths attributable to AMR could reach 2 million in 2050
This past Monday (November 18) marked the beginning of the annual World Antimicrobial Resistance (AMR) Awareness Week. According to the WHO, AMR occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines, making infections harder to treat and increasing the risk of disease spread, severe illness and death. This often happens as a consequence of drug resistance, making antibiotics and other medical interventions less effective or even totally ineffective against new infections and viruses. Medical experts estimate that global deaths attributable to AMR could reach almost 2 million in 2050. Cumulatively, the world could see over 39 million deaths due to AMR between 2025 and 2050. The elderly appear to be particularly vulnerable to this issue, with AMR-related deaths rising by over 80 per cent among those older than 70 years between 1990 and 2021. South Asia, Latin America and the Caribbean are the regions most affected by the problem. It is not a coincidence that the problem is worse in the Global South. While access to medical interventions like antibiotics has improved, this access is often very poorly regulated, if at all. Pakistan, where antibiotic consumption is the third highest in the world, is notorious for how easily one can obtain drugs or medications without a prescription and doctors who recklessly administer antibiotics without a proper diagnosis.
This is exactly the sort of situation in which drug resistance and AMR can be expected to thrive, with some studies estimating that AMR led to over 200,000 deaths in 2019 alone. The lesson to absorb during this week is that medicine, without proper oversight and usage, can become an enemy of good health. This is going to be hard to achieve in a country where people have begun reflexively reaching for antibiotics every time they fall ill and have an unending supply of pharmacies willing to give them the drugs they want without any prescription and even doctors willing to write one regardless of whether or not the patient really needs one. In fact, one can safely guess that most people in Pakistan are not even aware that reckless use of antibiotics and other drugs can indeed be a problem. Most of our public health woes tend to be rooted in a lack of awareness and misinformation.
When it comes to AMR, a lack of awareness basically means a nation sleepwalking into the next major pandemic. A superbug resistant to all kinds of medical interventions is something the country simply cannot afford. And given the increasingly interconnected nature of different regions, poor oversight over drug usage in some regions is something the whole world must be concerned about. Solving the problem starts with making sure people cannot simply acquire powerful antibiotics whenever they want and that doctors only prescribe certain drugs when they are absolutely certain that their patients need them.
-
 Record Set Straight On King Charles’ Reason For Financially Supporting Andrew And Not Harry
Record Set Straight On King Charles’ Reason For Financially Supporting Andrew And Not Harry -
 Michael Douglas Breaks Silence On Jack Nicholson's Constant Teasing
Michael Douglas Breaks Silence On Jack Nicholson's Constant Teasing -
 How Prince Edward Was ‘bullied’ By Brother Andrew Mountbatten Windsor
How Prince Edward Was ‘bullied’ By Brother Andrew Mountbatten Windsor -
 'Kryptonite' Singer Brad Arnold Loses Battle With Cancer
'Kryptonite' Singer Brad Arnold Loses Battle With Cancer -
 Gabourey Sidibe Gets Candid About Balancing Motherhood And Career
Gabourey Sidibe Gets Candid About Balancing Motherhood And Career -
 Katherine Schwarzenegger Shares Sweet Detail From Early Romance Days With Chris Pratt
Katherine Schwarzenegger Shares Sweet Detail From Early Romance Days With Chris Pratt -
 Jennifer Hudson Gets Candid About Kelly Clarkson Calling It Day From Her Show
Jennifer Hudson Gets Candid About Kelly Clarkson Calling It Day From Her Show -
 Princess Diana, Sarah Ferguson Intense Rivalry Laid Bare
Princess Diana, Sarah Ferguson Intense Rivalry Laid Bare -
 Shamed Andrew Was With Jeffrey Epstein Night Of Virginia Giuffre Assault
Shamed Andrew Was With Jeffrey Epstein Night Of Virginia Giuffre Assault -
 Shamed Andrew’s Finances Predicted As King ‘will Not Leave Him Alone’
Shamed Andrew’s Finances Predicted As King ‘will Not Leave Him Alone’ -
 Expert Reveals Sarah Ferguson’s Tendencies After Reckless Behavior Over Eugenie ‘comes Home To Roost’
Expert Reveals Sarah Ferguson’s Tendencies After Reckless Behavior Over Eugenie ‘comes Home To Roost’ -
 Bad Bunny Faces Major Rumour About Personal Life Ahead Of Super Bowl Performance
Bad Bunny Faces Major Rumour About Personal Life Ahead Of Super Bowl Performance -
 Sarah Ferguson’s Links To Jeffrey Epstein Get More Entangled As Expert Talks Of A Testimony Call
Sarah Ferguson’s Links To Jeffrey Epstein Get More Entangled As Expert Talks Of A Testimony Call -
 France Opens Probe Against Former Minister Lang After Epstein File Dump
France Opens Probe Against Former Minister Lang After Epstein File Dump -
 Last Part Of Lil Jon Statement On Son's Death Melts Hearts, Police Suggest Mental Health Issues
Last Part Of Lil Jon Statement On Son's Death Melts Hearts, Police Suggest Mental Health Issues -
 Leonardo DiCaprio's Girlfriend Vittoria Ceretti Given 'greatest Honor Of Her Life'
Leonardo DiCaprio's Girlfriend Vittoria Ceretti Given 'greatest Honor Of Her Life'