Women face double risk of death after heart attack compared to men: study
Younger women, aged 55 and below, experienced delays in receiving treatment upon arrival at the hospital
A study recently covered by The Independent discovered a concerning gender disparity in post-heart attack mortality rates, revealing that women face double the risk of death compared to men. The researchers behind the study stressed the importance of raising awareness about the specific risks women face when it comes to heart disease.
In addition to the increased mortality risk, the study found that younger women, aged 55 and below, experienced delays in receiving treatment upon arrival at the hospital. They had to wait approximately 15 minutes longer than men for medical intervention, potentially exacerbating the severity of their condition.
Another notable finding from the study demonstrated that women with a fully obstructed coronary artery experienced a worse prognosis during their hospital stay compared to men. Dr Mariana Martinho, the lead author of the study, emphasised that women of all ages who suffer from a heart attack are particularly vulnerable to poor outcomes. To improve these outcomes, she recommended regular monitoring, strict control of blood pressure, cholesterol levels, and diabetes, as well as referral to cardiac rehabilitation programs.
The study also shed light on other disparities between men and women in the aftermath of an ST-elevation myocardial infarction (STEMI). Researchers specifically examined the differences in outcomes between premenopausal and postmenopausal women. The study involved 884 participants, with women accounting for 27% of the cohort, and the average age being 62 years.
Results showed that women had higher rates of high blood pressure, diabetes, and prior strokes compared to men. Additionally, premenopausal women experienced longer wait times for treatment upon hospital arrival when compared to men. After considering various factors such as diabetes, high cholesterol, hypertension, coronary artery disease, heart failure, chronic kidney disease, peripheral artery disease, stroke, and family history of coronary artery disease, adverse outcomes were compared between genders.
Within 30 days, 11.8% of women had died compared to 4.6% of men, and at the five-year mark, 32.1% of women had died compared to 16.9% of men. Furthermore, women experienced a higher incidence of major adverse cardiovascular events over the course of five years compared to men.
Dr Martinho emphasised that women faced a two to three times higher likelihood of adverse outcomes in the short and long term, even after adjusting for other conditions and receiving the percutaneous coronary intervention (PCI) within the same timeframe as men. She concluded that these findings reinforce the urgent need for increased awareness of the risks of heart disease in women.
-
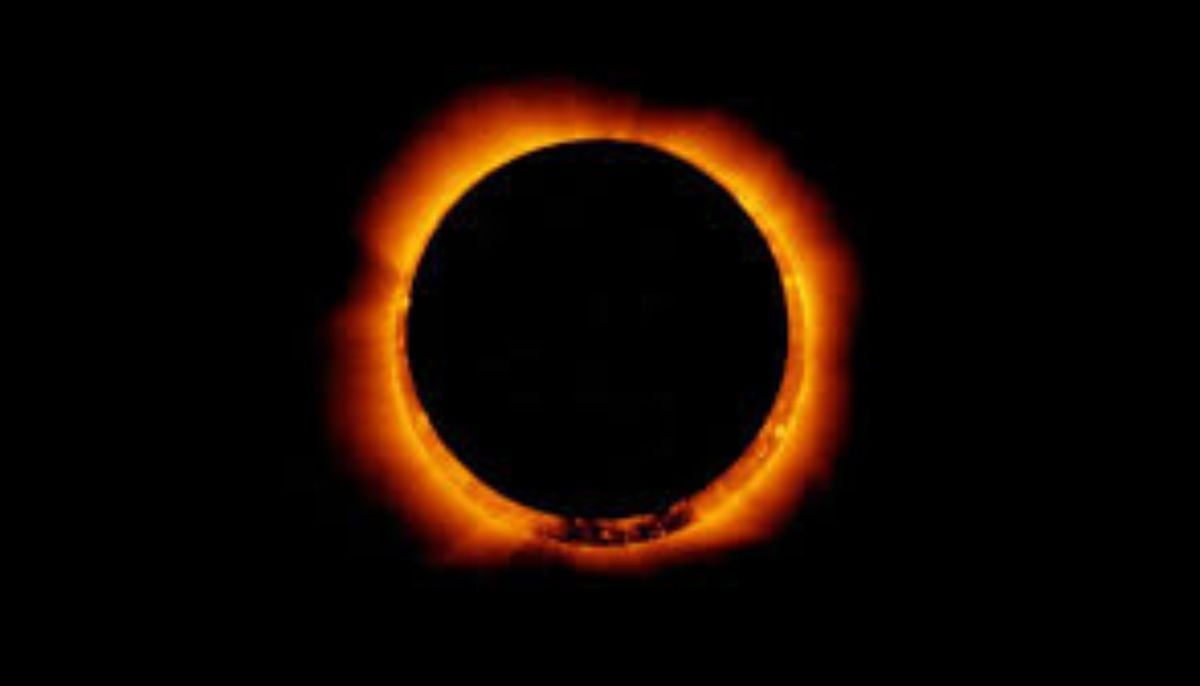
Annular solar eclipse 2026: Where and how to watch ‘ring of fire’
-
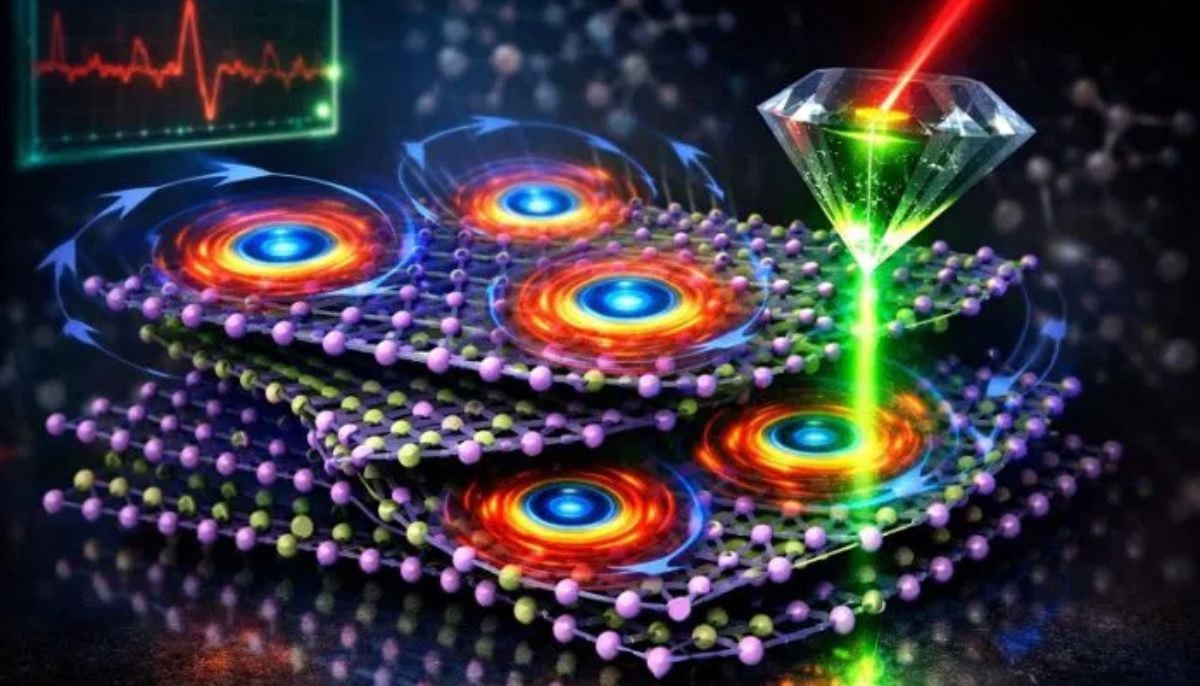
Scientists discover rare form of 'magnets' that might surprise you
-
Humans may have 33 senses, not 5: New study challenges long-held science
-
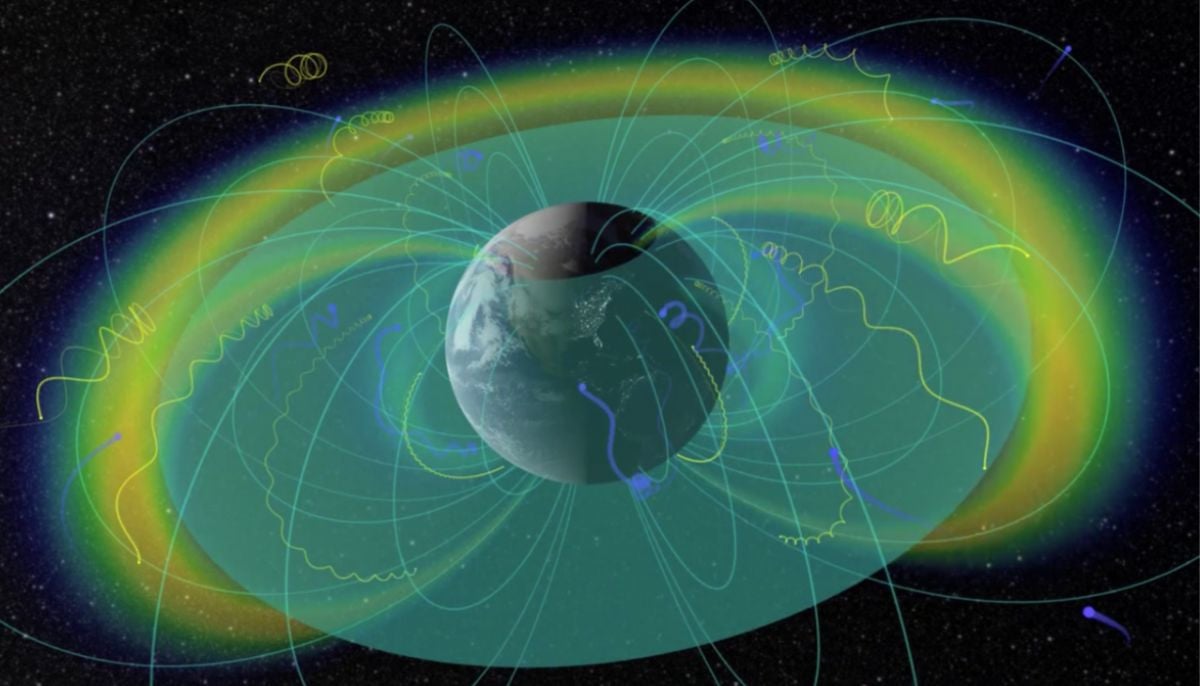
Northern Lights: Calm conditions persist amid low space weather activity
-
SpaceX pivots from Mars plans to prioritize 2027 Moon landing
-
Dutch seismologist hints at 'surprise’ quake in coming days
-
SpaceX cleared for NASA Crew-12 launch after Falcon 9 review
-
Is dark matter real? New theory proposes it could be gravity behaving strangely