Pakistan needs integrated emergency care systems, say experts
The global Disease Control Priorities Project estimates that nearly half of deaths and over a third of disability in low- and middle-income countries can be addressed by the implementation of effective emergency care.
“The solution is to establish integrated emergency and trauma care systems with pre- and post-emergency department care nationwide,” said Dr Junaid Razzak, director of the Centre for Global Emergency Care and professor of emergency medicine and international health at the Johns Hopkins University School of Medicine.
Dr Razzak was the keynote speaker on Friday at the inaugural ceremony of the Aga Khan University’s 21st National Health Sciences Research Symposium that is focusing, this year, on ‘emergency care: time and life matter’.
He recalled how he played a vital role in the establishment of emergency medicine as a specialty in Pakistan and became the founding chair of the department of emergency medicine at AKU – his alma mater – in 2008.
“Although College of Physicians and Surgeons Pakistan recognised emergency medicine as a specialty in 2011, there are not more than nine qualified emergency medicine specialists in the country today. Studies have also found significant gaps in the availability of essential resources, accessibility, patient-centricity and staff training,” said Dr Razzak.
“This is an alarming situation in the country with a population of over 220 million. The impact on saving lives can only be achieved through a health system that is sponsored by the state with support from public and private institutions.”
He stated that emergency care demands highly functional integrated health system, and complex and prompt care decisions. “We need a multi-prong strategy: predict the potential path of emergency care development if we follow the trajectory followed by the high income, more developed countries; and explore how new technologies such as telemedicine, artificial intelligence and machine learning can augment and impact the future of emergency care in low resource settings.”
He stressed that emergency departments should aim to provide a safe, committed, compassionate and caring service.
“AKU and other academic institutions in Pakistan can play a significant role in developing and testing innovations for futuristic emergency care system,” he added.
The second keynote speaker was Dr Scott Newton, a graduate of the Johns Hopkins University’s Doctor of Nursing Practice programme and the vice president of Care Model Solutions.
“Globally, emergency medicine is innovating to meet the demands of a growing population for care,” said Dr Newton. “Increased demands do require an agile workforce ready for high-touch and high-tech practice.”
“A well-established emergency care system can help achieve the United Nations’ Sustainable Development Goals: Goal 3 on good health and well-being; Goal 11 on sustainable cities and communities; and Goal 16 on peace, justice and strong institutions,” said Dr Asad Mian, head of the organising committee and the chair of AKU’s department of emergency medicine, in his welcoming address. “Overall, good emergency care can improve outcomes in no less than 10 SDG targets,” he said.
On the occasion, Dr David Arthur, dean of AKU’s School of Nursing and Midwifery, and Dr Mushtaq Ahmed, interim dean of the Medical College; and Hans Kedzierski, chief executive officer of the Aga Khan University Hospital, also addressed the audience.
The symposium is to continue till November 11. The second day will cover discussions on women in medicine, emergency medicine development in Pakistan, moral dilemmas in emergencies, ‘Ignite EM All’, and several other sessions.
‘Igniters’ speak their mind
Imagine a child receiving a “pain-free invisible” injection at an emergency department. The needle is hidden in a watch-like device with a hollow dial and a local anaesthetic at its base numbs the area of the needle’s insertion, thus making it pain-free.
The idea is the brainchild of Mir Ibrahim Sajid, a third-year student at the Aga Khan University’s Medical College, and one of the six presenters at an Ignite session – part of AKU’s 21st National Health Sciences Research Symposium that is focusing, this year, on ‘emergency care: time and life matter’.
Ignite, a speedy presentation series with just five minutes for 20 slides, is organised by AKU’s Critical Creative Innovative Thinking forum and is intended to light a spark in the audience to think differently.
Sajid continued, “Given that patients, especially young patients, are often miserable in an emergency department, there is a chance that the needle might be dislocated from its position, leading to the skin becoming inflamed.”
“So this device, pain-free invisible needle or PFIN, has an additional feature, a small chipset of a gyro sensor that records rotational movement of the watch. So when the recorded angular rotation is greater than a pre-fixed value, the chipset will send a signal to the nursing station to check the needle’s position,” explained the young entrepreneur while pitching his idea to potential investors.
Ume-e-Aiman Chhipa, a graduate of Dow Institute of Physical Medicine and Rehabilitation, shared the idea of red stripes from a hospital’s main gate all the way to the emergency department.
“Many people have lost their loved ones just because they couldn’t read signs or understand right-left paths well enough to find their way to the emergency department in a timely fashion,” she lamented. “Red stripes or a GPS solution should take them directly to the emergency department.”
Maheen Khan, a final-year student and Mehek Narmeen, a third-year student both from Dow Medical College, told the story of a student-run project First Response Initiative of Pakistan to teach first responders across the country how to react in an emergency, and to work towards a mass disaster task force for Karachi.
Earlier on the second day of the symposium, Dr Adnan Hyder, senior associate dean for research and professor of global health at the Milken Institute School of Public Health, George Washington University, talked about moral dilemmas in emergencies and challenges in applied ethics.
“Research is an integral component of emergency medicine as it allows improvements in care for the patient and for the system,” said Dr Hyder. “However, it is the responsibility of emergency care providers to consider ethical obligations while conducting research in the emergency room and the role of ethics committees to help create safe systems for learning in critical areas.”
In her talk, Dr Barbra Villona, an international emergency physician and American College of Emergency Physicians’ ambassador to Pakistan, explained what the current evidence showed about physician gender bias and why it needed to be addressed.
“Gender bias has created a gap in medicine but it is not a gap between men and women. It is a gap between where we are and where we need to be,” said Dr Villona.
Dr Taj Hassan, consultant in emergency medicine at the Leeds Teaching Hospitals NHS Trust and president of the Royal College of Emergency Medicine, UK, talked about building a collaborative road for emergency medicine development in Pakistan, via a video link.
Other speakers of the day included Dr Nick Brown, a paediatrician and epidemiologist at the International Centre for Maternal and Child Health, Sweden, who has been closely affiliated with the Department of Paediatrics and Child Health at AKU for several years; Dr Desmond Mao, an emergency physician at Khoo Teck Puat Hospital, Singapore; and Dr Nathan S. Bryan, a molecular medicine expert, from Baylor College of Medicine, Houston, Texas. The symposium will continue till November 11. The concluding day will cover discussions on impacting paediatric emergency care in Sindh, instilling creativity and innovation for the child in the emergency department, and school preparedness for emergencies.
-
 Apple Sued Over 'child Sexual Abuse' Material Stored Or Shared On ICloud
Apple Sued Over 'child Sexual Abuse' Material Stored Or Shared On ICloud -
 Nancy Guthrie Kidnapped With 'blessings' Of Drug Cartels
Nancy Guthrie Kidnapped With 'blessings' Of Drug Cartels -
 Hailey Bieber Reveals Justin Bieber's Hit Song Baby Jack Is Already Singing
Hailey Bieber Reveals Justin Bieber's Hit Song Baby Jack Is Already Singing -
 Emily Ratajkowski Appears To Confirm Romance With Dua Lipa's Ex Romain Gavras
Emily Ratajkowski Appears To Confirm Romance With Dua Lipa's Ex Romain Gavras -
 Leighton Meester Breaks Silence On Viral Ariana Grande Interaction On Critics Choice Awards
Leighton Meester Breaks Silence On Viral Ariana Grande Interaction On Critics Choice Awards -
 Heavy Snowfall Disrupts Operations At Germany's Largest Airport
Heavy Snowfall Disrupts Operations At Germany's Largest Airport -
 Andrew Mountbatten Windsor Released Hours After Police Arrest
Andrew Mountbatten Windsor Released Hours After Police Arrest -
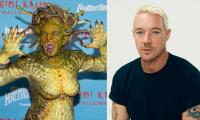 Heidi Klum Eyes Spooky Season Anthem With Diplo After Being Dubbed 'Queen Of Halloween'
Heidi Klum Eyes Spooky Season Anthem With Diplo After Being Dubbed 'Queen Of Halloween' -
 King Charles Is In ‘unchartered Waters’ As Andrew Takes Family Down
King Charles Is In ‘unchartered Waters’ As Andrew Takes Family Down -
 Why Prince Harry, Meghan 'immensely' Feel 'relieved' Amid Andrew's Arrest?
Why Prince Harry, Meghan 'immensely' Feel 'relieved' Amid Andrew's Arrest? -
 Jennifer Aniston’s Boyfriend Jim Curtis Hints At Tensions At Home, Reveals Rules To Survive Fights
Jennifer Aniston’s Boyfriend Jim Curtis Hints At Tensions At Home, Reveals Rules To Survive Fights -
 Shamed Andrew ‘dismissive’ Act Towards Royal Butler Exposed
Shamed Andrew ‘dismissive’ Act Towards Royal Butler Exposed -
 Hailey Bieber Shares How She Protects Her Mental Health While Facing Endless Criticism
Hailey Bieber Shares How She Protects Her Mental Health While Facing Endless Criticism -
 Queen Elizabeth II Saw ‘qualities Of Future Queen’ In Kate Middleton
Queen Elizabeth II Saw ‘qualities Of Future Queen’ In Kate Middleton -
 Amanda Seyfried Shares Hilarious Reaction To Discovering Second Job On 'Housemaid': 'Didn’t Sign Up For That'
Amanda Seyfried Shares Hilarious Reaction To Discovering Second Job On 'Housemaid': 'Didn’t Sign Up For That' -
 Hilary Duff Reveals Deep Fear About Matthew Koma Marriage
Hilary Duff Reveals Deep Fear About Matthew Koma Marriage



